Resilience and Reinvention: Preparing for the Global Age Wave with a North Star Vision
At the ADvancing States HCBS Conference in Baltimore (August 2025), the Aging Policy Intensive session delivered a powerful message: the U.S. is standing at the threshold of an aging transformation, and “business as usual” will not get us where we need to go.
Moderator Abby Cox (ADvancing States) hosted a series of leaders including:
Ursel J. McElroy, Director, Ohio Department of Aging
Susan DeMarois, Director, California Department of Aging
Nels Holmgren, Division Director, Utah Division of Aging and Adult Services
With reflections from Jackie from Minnesota on oversight and accountability
Together, they painted a picture of what lies ahead: a future shaped by demographics, strained by trust gaps, and fueled by opportunities for innovation.
Aging as a National Transformation
Director Ursel McElroy opened with a sweeping global view:
By 2040, the world’s older adult population will reach 1.3 billion.
In the U.S., older adults will number 71 million, nearly 20% of the population.
For the first time in history, there will be more older adults than children.
This shift is not a regional issue — it is a national transformation with profound implications for:
Communities: Urban planning, housing, transportation.
Healthcare: From acute care to long-term supports.
Economies: Strains on labor markets and dependency ratios.
McElroy reminded us: “Aging is a megatrend, and we are on the front lines.”
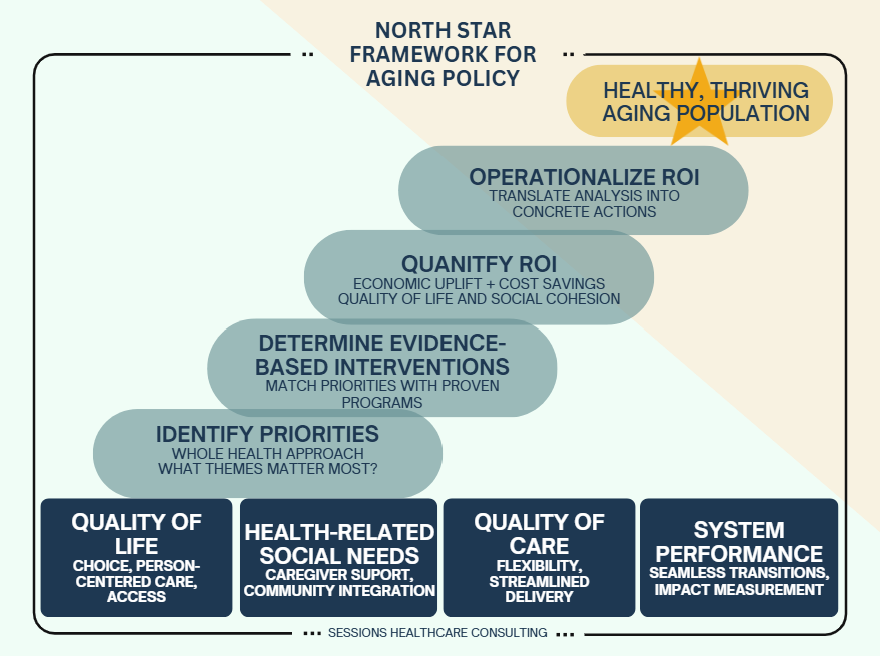
The Ohio Framework: Anchoring in a North Star
Ohio has structured its journey around four road stops:
Identify priorities — a whole-health approach that goes beyond clinical care.
Determine evidence-based interventions — align programs with proven strategies.
Quantify return on investment (ROI) — measure both economic and quality-of-life impacts.
Operationalize ROI — move from analysis to action.
The state’s four pillars of aging reform are:
Quality of life (choice, person-centered care, access)
Health-related social needs (navigation, caregiver support, community integration)
System performance (seamless transitions, measurement)
Quality of care (flexibility, streamlined delivery)
Ohio’s Path to a North Star Vision for Aging
At the top sits the North Star Goal: A healthy and thriving aging population.
Supporting this vision is a four-step pathway. Beneath the pathway are the Four Pillars of the Foundation. Put together, the structure conveys pillars at the base, a pathway of strategic steps, and a guiding North Star above.
Ohio has also invested in dashboards to transform raw data into action:
A public Long-Term Care Quality Navigator (100k+ users).
An internal powerhouse dashboard that ingests 22 million data points across 200+ metrics.
These tools help Ohio leaders “zoom out” from daily pressures to see the larger significance — and they have already been nationally recognized.
Trust, Oversight, and the Shadow of Fraud
Jackie from Minnesota brought a sobering reminder: with money comes responsibility. She referenced the largest COVID-19 fraud scheme in the nation (“Feed Our Future”), which resulted in $250M in losses and dozens of indictments【Justice.gov†source】.
The fallout has forced states like Minnesota to overhaul their monitoring and accountability systems. Legislatures now demand new manuals, new audits, and more robust oversight to rebuild public trust.
The message was clear: trust is as important as funding. Without it, every innovation risks being overshadowed.
California: Communication as Policy
Susan DeMarois described how California has invested not only in services but in communication strategies that meet older adults where they are.
Highlights include:
Aging in California Guide (link) — a resource tailored to diverse communities.
Campaigns like “Just Ask” and “Start the Conversation” to encourage older adults to seek help and families to engage.
Tools for older adult behavioral health and emergency preparedness.
California has learned that different populations require different channels:
Tribal and rural communities: Word of mouth and hyperlocal networks.
Urban centers: Broader campaigns to reach those who may feel lost in the crowd.
Caregivers (avg age 47): Social media outreach.
Older adults themselves: Printed materials remain critical.
Accessibility is non-negotiable: captioned videos, alt-text, plain language, QR codes. As DeMarois put it, “All communication must be accessible — or it’s not communication at all.”
Utah: Reinvention Through Restructuring
Utah has undergone a major reorganization, merging its Department of Health and Department of Aging into a single Department of Health and Human Services.
According to Nels Holmgren, this merger created opportunities:
New collaborations across child, youth, medical, and disability services.
Results-Based Accountability (RBA): Programs are judged not just by activity but by whether lives are actually improved.
GRIT (Government Reform Initiative and Transparency): Designed to end practices that “aren’t helping” and focus on what works.
Holmgren stressed that innovation isn’t always voluntary. Sometimes change is thrust upon agencies, and resilience is measured by the ability to find the silver linings.
The Hard Questions
Throughout the session, a recurring theme emerged: leadership requires making hard choices.
What is our North Star for aging policy?
What evidence supports the interventions we believe in?
Are we prepared to release tightly held beliefs if the data tells a different story?
How do we balance savings tomorrow with scarce dollars today?
Which programs can be reshaped, consolidated, or even sacrificed to fund higher-impact strategies?
McElroy called this the “whack-a-mole” reality of public budgeting: every new program risks crowding out another. Leaders must weigh tradeoffs deliberately, without losing sight of the larger vision.
Shared Themes Across States
Despite their different contexts, three themes cut across the presentations:
Aging is everyone’s issue.
Urban planning, parks, transportation, housing — all are aging policy, whether they recognize it or not.Data and ROI are the future.
From Ohio’s dashboards to Georgia’s respite ROI study (every $1 returns $1.40), the ability to quantify outcomes will determine which programs survive.Communication builds trust.
California’s outreach, Minnesota’s audit overhaul, and Utah’s RBA all highlight that credibility is fragile. Without trust and transparency, no program endures.
My Reflection
This intensive session left me with both urgency and hope.
Urgency, because the demographic wave is real. By 2040, aging will reshape our labor force, health systems, and economies. Business as usual will fail.
Hope, because leaders across states are already reinventing, reframing, and embracing risk. They are building dashboards, launching communication campaigns, restructuring agencies, and facing down fraud.
As I see it, the road ahead requires three commitments:
Anchor in a North Star vision — define what healthy aging means for your state or community.
Invest in evidence and ROI — not just what we believe will work, but what data proves works.
Rebuild and maintain trust — with the public, with providers, and with workers.
Aging is a megatrend. It will not wait for us to get comfortable. But if we are willing to be bold, collaborative, and data-driven, we can shape a future where longevity truly means a good life, not just a long one.