Looking Ahead: Forecasting State and Federal Policy Trends in HCBS and Aging Services
The 2025 ADvancing States HCBS Conference in Baltimore closed with both optimism and realism. Participants celebrated what states, providers, and caregivers have accomplished—but also recognized that the hardest work lies ahead. If there was one unifying sentiment, it was this: change is accelerating, and the systems that anticipate it will be the ones that thrive.
Here are the policy trends on the horizon that stakeholders must watch as HCBS, aging, and workforce policy evolve.
1. The New HCBS Waiver Option: Shifting the Eligibility Landscape
The One Big Beautiful Bill Act (OBBB) created a new 1915(c) waiver option that removes the institutional level-of-care (LOC) requirement.
Effective July 2028, this option is designed to reduce waiting lists and serve populations who need support but do not meet strict LOC thresholds.
Expect TBI and other “middle need” populations to benefit most, while states weigh how to balance funding, staffing, and service arrays.
Early adopters will likely be states with long waiting lists and strong advocacy communities pushing for expanded eligibility.
Forecast: Pilot programs will begin as soon as FY26 dollars flow to CMS, but wide adoption won’t come until 2028. The states that start designing needs-based criteria now will be positioned to launch smoothly.
2. Community Engagement & Work Requirements: A New Layer of Complexity
OBBB also introduced Medicaid community engagement requirements, effective as early as 2026.
Adults aged 19–64 in certain waiver programs must meet 80 hours per month of work, education, or community service.
Exceptions exist for older adults, caregivers, and medically frail populations, but states will shoulder the administrative burden of eligibility verifications every six months.
States must also build fair hearing processes and hardship waivers into their systems.
Forecast: Expect uneven implementation, legal challenges, and possible delays—but also operational strain on eligibility systems already stretched thin.
3. Aging Policy: From Siloed Programs to National Transformation
By 2040, the U.S. will have more older adults than children for the first time in history. States are experimenting with master plans for aging, but without alignment, risk remains high.
OAA reauthorization is stalled, but new regulations require states to update plans, submit corrective action plans, and comply with ACL guidance amidst significant staff reductions at the federal level.
States like Ohio and California are using dashboards, ROI models, and cross-agency coalitions to align investments with outcomes.
Forecast: Aging will move from a niche policy issue to a national economic and social priority within the decade. States that anchor efforts in evidence-based ROI models will have stronger cases for funding and political buy-in.
4. Direct Care Workforce: Universal Training and Credentialing
The workforce crisis was threaded through every session of the conference. With more than 8.9 million job openings expected by 2032, the call is for universal credentialing, portable training, and career ladders.
Wisconsin’s Certified Direct Care Professional (CDCP) model is leading the way, with microcredentials, virtual badges, and language access expansions.
Michigan’s IMPART Alliance is building competency-based standards and apprenticeship programs tied to policy recommendations.
Other states (CO, ND, TX) are testing registries and LMS platforms with shared-cost models.
Forecast: Expect a wave of state investments in training infrastructure in the next 3–5 years, with growing calls for a national model that establishes portability across states and settings.
5. Technology as a Force Multiplier—If Trust Can Be Built
From enabling technology pilots to job-matching platforms, the role of technology is growing. But cultural resistance remains a barrier.
Enabling Technology Engagement Network (ETEN) states are building proof-of-concept pilots to overcome “what if” fears from families, providers, and administrators.
Vendors are being urged to co-design with lived experience in mind—recognizing that adoption is highest when technology is relevant, simple, and trustworthy.
Forecast: Technology will be the differentiator for states facing workforce shortages, but adoption will lag unless paired with education, digital literacy, and a strong human touch.
6. Federal-State Tensions: Funding, Oversight, and Innovation
Federal funding is increasingly tied to strict oversight, short timelines, and political appointee review.
New rules require discretionary grants to include “termination for convenience” clauses, introducing instability for programs reliant on federal dollars.
States continue to struggle with Medicaid waiver neutrality, provider taxes, and state-directed payments under OBBB.
The rural health transformation fund ($10B annually) offers opportunity but requires plans by Dec 2025—putting states on the clock.
Forecast: The next decade will see sharper divides between states that seize federal funds with readiness and those that miss opportunities due to capacity gaps. Intermediaries—consultants, universities, and vendor partnerships—will play a key role in bridging those gaps.
7. Forecasting the Next Decade
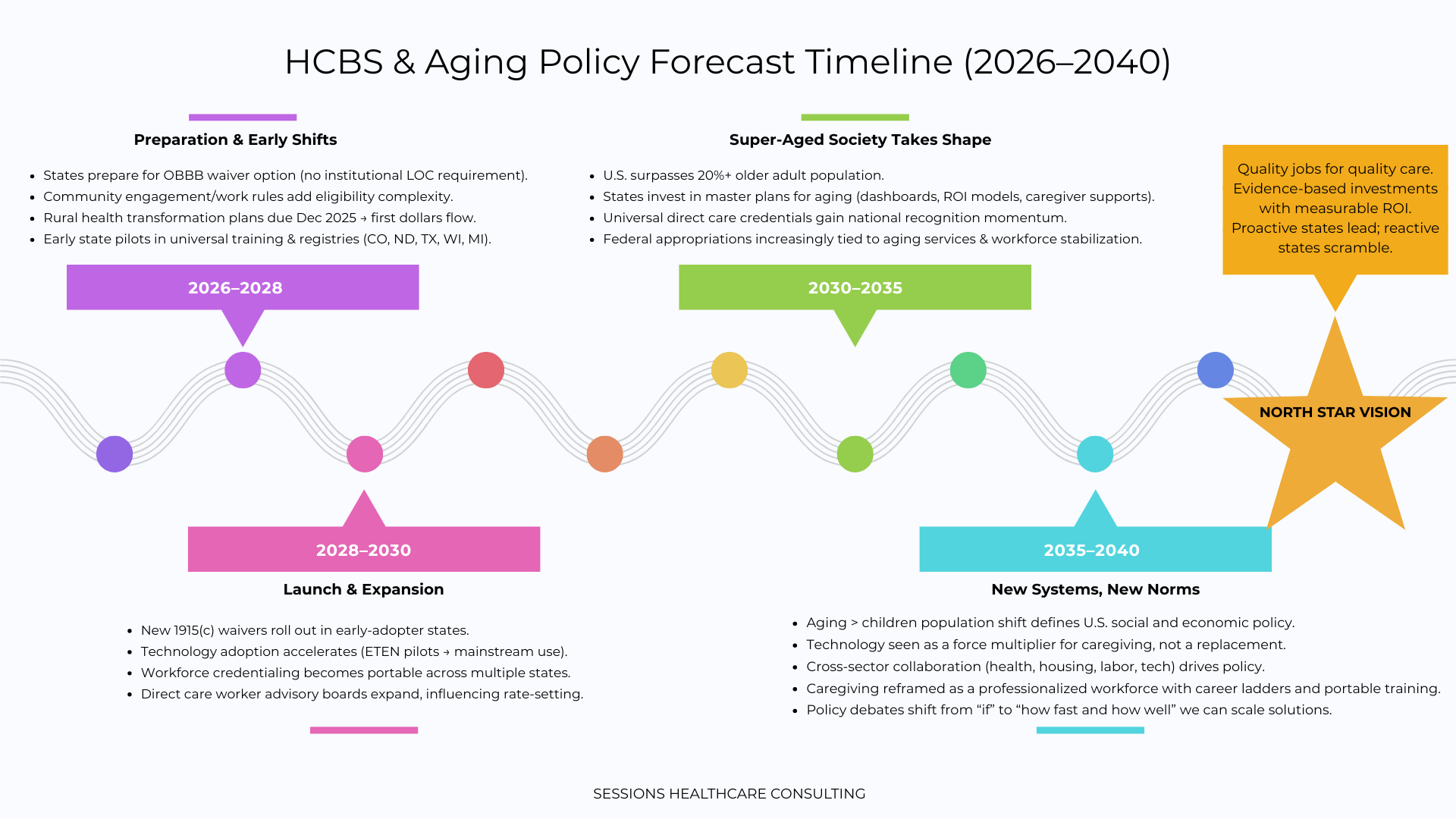
2026–2028: Heavy lift for states preparing for OBBB waiver, rural health transformation, and community engagement rules.
2028–2030: First wave of new waivers launches; universal training frameworks expand; technology adoption accelerates as workforce shortages deepen.
2030–2040: The “super-aged society” shift takes hold. Expect aging to dominate federal appropriations and state budgets, with caregiving redefined as a professional, credentialed workforce supported by technology and cross-sector planning.
Conclusion: From Trend-Spotting to Strategy
The 2025 HCBS Conference made one thing clear: the future is arriving faster than most systems are ready for. States, providers, and partners cannot afford to treat policy change as compliance alone.
The call is for proactivity, experimentation, and collaboration—to treat every waiver, every dashboard, every training program not as a box to check but as an opportunity to redefine how aging and disability services are delivered.
Those who wait will scramble and suffer. Those who lead will shape the next generation of care and redefine quality standards in American healthcare.